Farewell & Goodbye: Lessons Learned Over a Lifetime of Cost Estimating
June 30, 2025

Cullen S. Keen, AIA ACHA EDAC SEPS
The root of patient room design was drastically different than what we design today. The earliest hospitals were open wards intended to promote natural airflow through the space, creating narrow buildings with windows on either side. This was necessary without our modern mechanical ventilation systems, and that strategy is still a valid strategy in non-developed countries. In the early to mid-1900s, the open wards were broken into smaller rooms—whether private or semiprivate—but the footprint remained narrow double loaded corridors with nurse stations at key intersections. Older U. S. Department of Veterans Affairs hospitals often stretched the semiprivate arrangement to still include four-person wards.
Over the years, inpatient unit design has made many improvements. Decentralized models put the nurses and supplies closer to the patient to increase the time for direct patient care. Layouts and features reduce the risk of falls. Lighting is improved for both patient comfort and clinical treatment. Integrated patient service walls organize the power, data, and medical gases into much more aesthetically pleasing elements – with greater flexibility as well. The size of rooms is much greater than 50 years ago, affording more equipment in the room. Space is provided for family members to participate in the care of patients. The VA design guide for inpatient units acknowledges and encourages such improvements.
However, most inpatient beds are already built. Older VA buildings rarely support the best practices in inpatient unit design. Replacement bed tower projects are few and far between as they are costly, and they leave old towers that are difficult to convert into new functions. Most VA Medical Centers must rely on inpatient privacy renovations to improve the environment for our veterans, applying the improved design strategies where possible.
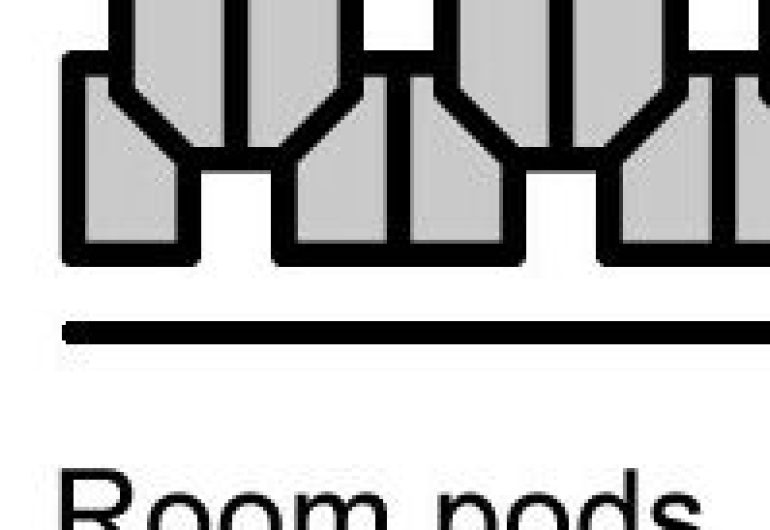
In the 1960s through 1980s, architects explored different shapes for inpatient units, testing triangular and radial shapes to maximize the number of patient rooms with windows that could encircle a small core. Pod configurations were developed to increase the number of rooms along the linear feet of corridor. Unfortunately, these shapes did not anticipate the growth in medical equipment and technology, and they limit the expandability and flexibility of the building.
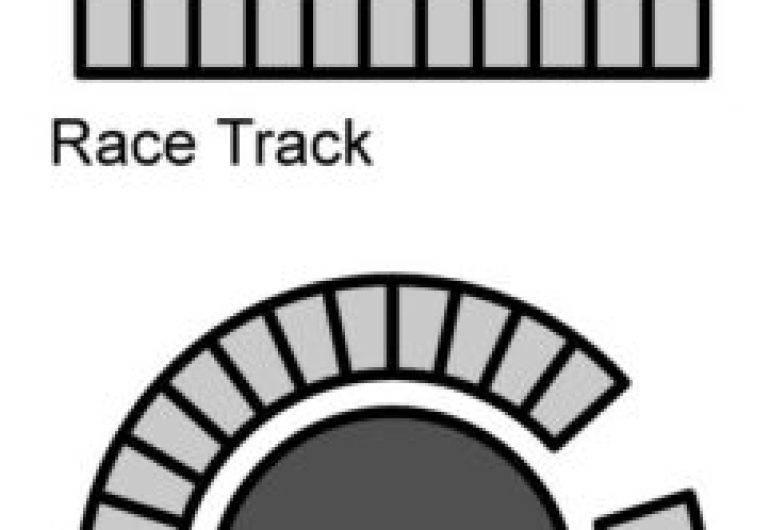
The most flexible inpatient units tend to be wider footprints with some version of a racetrack layout, providing more support space for the number of patient rooms. Today, most hospitals are designed with some variation of the racetrack layout. The size and shape of those racetrack cores can vary greatly, with architects applying design creativity customized for the specifics of a hospital campus.
For most of the 1900s, patient rooms allocated between 100 and 150 square feet per patient. Semiprivate rooms may have been 200 square feet plus a tiny bathroom, and Private rooms 150 square feet plus the bathroom. The current FGI guidelines do not require much more space, 120 square feet of clear floor area for a private patient room, but the requirement for it to be clear area does make a difference. Most inpatient rooms built over the past few decades have been substantially larger than those requirements. It is more common to have the patient rooms within the range of 280 to 360 square feet including the bathroom. The VA design guidelines call for 280 square feet in the patient room plus 60 square feet in the bathroom for a total of 340 square feet.
Patient rooms have several basic layout strategies, largely revolving around the location of the toilet. Inboard, outboard, in between, footwall, and headwall locations are all possibilities with advantages and disadvantages. Another consideration is same-handed rooms for reducing potential errors. That can be expounded into nested rooms that adjust the shape o be less rectangular to optimize the visibility of staff to the patient and views to the exterior while still letting the toilet be on the headwall for patient fall safety.
The VA hospitals have been built over the course of a century. They can have the full range of inpatient unit types and patient room types. However, with many of the VA hospitals built in the Hill Burton era of the 1940s and 1950s, the long double-loaded corridors with narrow footprints are common. The depth of these rooms from corridor to the exterior wall can be as little at 13-feet. Column bays are often only 20 or 24-feet wide with either two single-patient rooms or one foot-to-foot semiprivate room within that bay. This produces a challenge creating private patient rooms that meet current VA design guides. The guidelines are based on 24-feet deep, 15-foot-wide rooms. Neither of those dimensions can be achieved within such small existing column bays. How do we resolve this?
The solution must combine existing rooms, meaning a reduction in total patient room quantity. The method of combining rooms depends on the actual dimensions of the building. If the corridor-to-exterior dimension is very narrow, the room layout must completely deviate from the VA design guide. Apogee pursued this arrangement at the Durham VA Medical Center. The family zone and toilet zone must rotate away from the headwall. Usually, two existing rooms will convert into one new private patient room with this orientation.
If the existing building has a deeper footprint, closer to the twenty-four feet in the design guide, then the conversion will take either 3 existing rooms into 2 new rooms or 4 existing rooms into 3 new rooms. In these cases, the new patient rooms can match the VA design guide layout.
Despite the physical constraints common among VA hospitals, with careful planning it is possible to create new patient rooms that meet the current vision for patient centered care, improved safety, and healing environments. The effort begins with listening to the goals of the VA. It continues with analysis of the existing constraints and developing a common understanding of what can be achieved. Thoughtful communication between the design team and the VA stakeholders will lead to the most workable and beneficial solutions.