By Cullen S. Keen, AIA, ACHA, EDAC, SEPS
Healthcare Planner / Architect
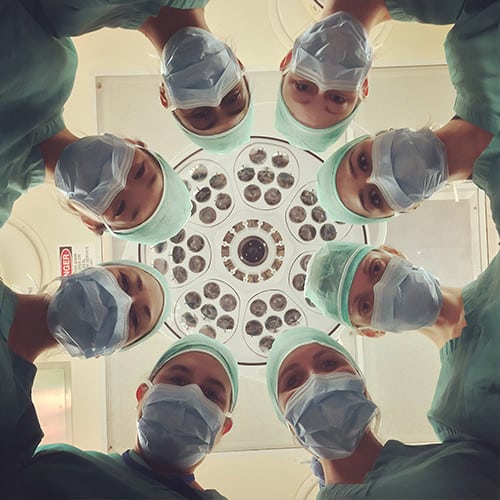
A key element of all hospitals is surgery. It is critical to patient care. It is the biggest money maker. And it is one of them most complex departments to design.
As the population continues to age and hospital visits become more acute, the surgery department must maximize effectiveness and efficiency, which brings us to the topic of flow. I use that term loosely – there are several types of flow being referenced.
First, there is patient flow. Good patient flow through the department improves throughput. It makes it easier to transport patients from pre-op to operating room to recovery. It makes the patients accessible to surgical staff that needs to check on recovering patients between surgeries.
Second, there is staff flow. How efficiently can staff get into the surgical suite? Are supplies readily accessible to reduce steps? Can staff see the procedure environment from the scrub station? Resolving these issues affords staff to get to the patient needs faster, thereby reducing turnaround time. Third, there is supply flow. How do sterile instruments and supplies enter the operating room? Are we minimizing risk of contamination?
Let’s look at some of the flow items to address:
- Convenient intake and discharge: For outpatient surgery, convenient access to pre-op and easy discharge from post-op is critical for patient satisfaction and minimizing wasted staff time for escorting.
- Flexibility for pre-op and post-op: While the purpose for pre-operative services and post-operative services differs, the spatial requirements are very similar. Organizing the two side by side or in parallel affords flexibility of shifting patient volume during peak times, allows support spaces to be shared, and permits staff to support one another.
- Clear in and out routes: Establish one-way flow from pre-op into the semi-restricted area and another route from the semi-restricted area to recovery. This will avoid delays waiting for another stretcher to move through a doorway or corridor.
- Discharge route: Patients do not always look their best when being discharged from surgery. Those patients may not want to be watched and the people in the waiting room probably don’t want to see them. For those reasons, it is best to develop a separate discharge route whenever possible. How separated that discharge is may vary. In some facilities, the route may be separate all the way to the vehicle. Other facilities may only be able to separate traffic past the waiting room, merging in the main corridor.
- Orientation of surgical table: The position of the surgical table within the operating room will differ for different procedures. However, one thing in universal: avoid circulating through the anesthesia zone. Operating room layout should define the functional zones of the room and create clear circulating routes around them.
- Pervasive handwashing locations: Handwashing is key for avoiding hospital acquired infections. Locating handwashing stations where they are in the normal paths of clinical staff and visitors encourages proper, frequent handwashing.
- Separating clean and soiled: While existing connections to other departments or spatial limitations may dictate certain routes, avoid crossing clean and soiled carts to protect the sterile integrity of the instruments.
- Immediate use sterilization: Current best practice is an immediate use sterilization (IUS) room positioned to allow the soiled instrument to be carried out of the operating room through the semi-restricted zone, cleaned in the IUS room, and returned to the operating room through the clean core.
- Air flow: Operating rooms require high air flow to reduce risk of hospital acquired infections. Air should flow from the ceiling above the patients toward low returns at the corners of the room, effectively flowing clean air over the patient and away from the sterile field. Combining laminar flow diffusers above the patient with linear air curtain diffusers ringing the sterile field provides the low velocity needed over the patient while also combating swirling of less clean air back into the sterile field.
Flow affects many broad healthcare issues, such as access to care, safety, patient satisfaction, and financial stability. Using an intelligent design process to address these topics can launch the project to a powerful solution supporting the mission of the healthcare organization.